GMS Current Topics in Otorhinolaryngology - Head and Neck Surgery 2013, Vol. 12, ISSN 1865-1011
Danger points, complications and medico-legal aspects in endoscopic sinus surgery
Werner Hosemann, C. Draf
Department of Otorhinolaryngology, Head and Neck Surgery, University of Greifswald, Germany
Summary
|
Localization / Type of Injury |
"Minor" Complication (5%) |
"Major" Complication (0.5% - 1%) |
|
orbita eye . optical nerve . optical muscle . nerves in orbita |
4.1 Damage of the lamina papyracea orbital emphysema (Lufteintritt), preseptal bleeding beneath the skin of the eyelid . . . . 4.7 Nerve injuries - infraorbital nerve, alveolar nerve |
5.1 Orbital haematoma Retrobulbar hematoma . 5.3 Reduced vision, visual field defects 5.4 Diplopia 5.5 enophthalmos (Zurückziehen des Augapfels) 5.6 Lacrimal duct injury complications in dacryocystorhinostomy |
|
mucosa |
4.2 Uncomplicated bleeding of the mucosa |
|
|
CSF Intracranial |
4.3 Uncomplicated liquorrhea (e.g. thru fistulae) ... can lead to major complications -> |
5.7 Skull base injury, tension pneumocephalus, encephalocele (Nach-Außen-Wölben von Hirnteilen) 5.8 Meningitis, brain abscess, intracranial haemorrhage 5.9 Direct mechanical cerebral trauma, severe combined injuries |
|
maxillary sinus middle meatus middle turbinate olfactory mucosa |
"missed ostium sequence", unstable middle turbinate with lateralisation . |
. . . 5.11 Anosmia |
|
olfactory region |
4.5 Hyposmia |
|
|
|
4.6 Atrophic rhinits |
|
|
Bleeding |
|
5.2 Injury of (*) anterior ethmoidal artery (*) posterior ethmoidal artery (*) sphenopalatine artery (*) internal carotid artery |
1 Preface
...
Furthermore, endonasal surgery has undergone an enormous expansion of its reach and its indications [40], [41] in specialized centers with continued development of 'simultaneous neuro-rhinosurgery' [21] and 'endoscopic rhino-neurosurgery'
2 Special aspects in endoscopic surgery of the paranasal sinuses
From the patients perspective endonasal surgery for chronic rhinosinusitis can be considered effective [44]. As compared to its "effectiveness" its application regarding formal evidence of standards is far from being beyond critical discussion:
....
3 Classification of complications in endonasal sinus surgery
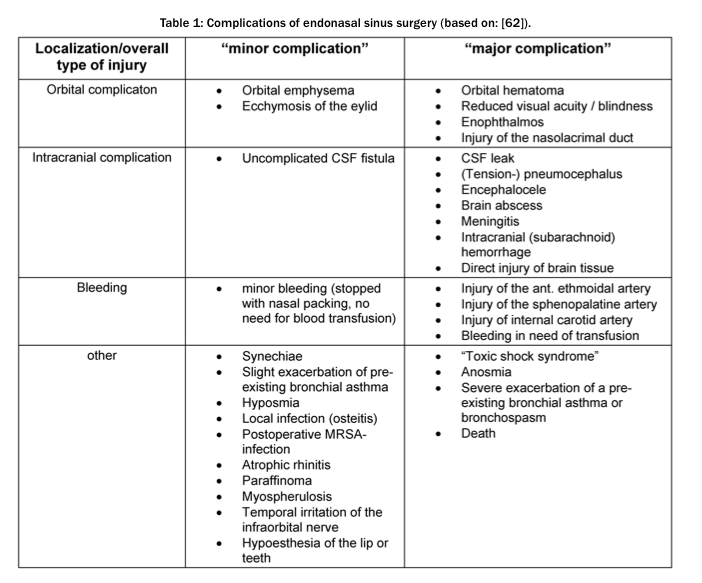
In general, sinus surgery has a relevant risk potential [61], [64]. When surgical errors occur in a rare case, the risk resulting in relevant physical damage is above average [65].
Doubtlessly, many patients with chronic rhinosinusitis are already burdened heavily simply due to their illness [66]. In other cases an unfavorable ratio results, with respect to the listed mistakes:
The risk potential is higher in transnasal endoscopic rhinoneurosurgery; altogether this accounts for approximately 10% (-25%) of complications. The reported numbers have to be discussed; these apply to heterogenic interventions and patients.
It can be assumed in each case that the values are below those of traditional craniofacial surgery [101], [102].
The otorhinolaryngologist as partner in a rhino-neurosurgical team is confronted with a significantly wider spectrum of possible errors and risks during surgery. Examples are:
Begriffserklärung:
emphysema: Eindringen von Luft
ecchymosis: kleinere Hautblutung
enophthalmos: Zurückziehen des Augapfels
CSF fistula: äußere Fistel der Subarachnoidalräume:
Arachnoidea = Kurzbez. für die zarte, gefäßarme, bindegewebige, beidseits endothelbedeckte mittlere Gehirn- u. Rückenmarkshaut
Synechia: fibröse Verklebung zweier normalerweise getrennter Gewebsschichten
Hyposmia: herabgesetzte Geruchsempfindung; s.a. Anosmie, Kakosmie
Anosmie: hochgradige Minderung bis Aufhebung der Geruchswahrnehmung, evtl. nur für bestimmte Riechstoffe (= elektive A. = Merosmie)
MRSA: multi-resistente staphylococcus aureus
atrophische Rhinitis: Gewebsschwund-bedingte Rhinitis
Rhinitis: Nasenschleimhautentzündung
Myospherulosis (also called spherulocytosis,[1]) is a foreign body-type granulomatous reaction to lipid-containing material and blood
scarring: Schrumpfen
If data from the "beginning international phase" ("surgical innovation adoption curve" [85]) of endoscopic surgery (such as 1988 to 1998) is excluded, endoscopic surgery displays a comparable safe procedure according to the subsequent comparison of literature [80]. The complication rate has globally decreased slightly during the past few years [14].
The risk of a complication increases under the following circumstances [38], [39], [61], [62], [63], [68], [74], [76], [86], [87], [88], [89], [90], [91], [92]:
Almost every one of the risk indicators mentioned in literature is subject to controverse discussions:
4 "Minor" complications
4.1 Damage of the lamina papyracea - orbital emphysema, preseptal bleeding
4.2 Uncomplicated bleeding of the mucosa
4.3 Uncomplicated liquorrhea
In general, localized cerebrospinal fluid fistulas cannot always be avoided, even when the procedure is carried out very carefully [264].
Epidemiology
Small and isolated CSF fistulas, which are treated at once successfully, count statistically as "minor complication" [68].
Diagnosis
Every patient that complains of severe headaches needs to be examined thoroughly [76].
... Regarding CT scans the quality of the image is crucial, reconstructed coronal planes frequently lead to misinterpretations [199], [209].
Under ideal conditions
In individual cases subclinical fistulas were detected with fluorescein, neither with beta trace nor with beta 2 transferrin [217]. Nevertheless even fluorescein has a limited sensitivity (74%-96%).
False-negative samples may occur, among others, due to a temporary blockage of the fistula through
In case of suspecting a false-negative result after injection, nasal packing is to remain for a certain amount of time, which later is checked for fluorescein [194].
Surgical management
Iatrogenic cerebrospinal fluid fistulas are usually below 3mm in size, in some cases 2-20 mm [192], [226], [227].
This recommendation is based on observations in traumatology [229] and on experience that only in 1/3 of cases with conservative treatment the scar is rigid enough [228].
Closure of cerebrospinal fluid leaks via endoscopic endonasal approach belongs to the standard repertoire of sinus surgery. There are various approved techniques for repairing defects [205], [226], [230]. The choice of approach does not necessarily influence whether the rhinorrhea ceases when applying the usual diligence [191]. In general,
may be used.
Autogenous transplants include mucosa, bone, cartilage, fat, fascia or mucoperichondrium. For matter of stabilization gelatin, cellulose or fibrin glue may be prepared in different ways [231].
The initial exposition of the defect is important. The area of the skull base defect needs to be "cleaned" from mucosa remnants and is prepared for the closure. If the leak is not easily identified, it may help to tilt the patient's head low and to ask the anesthesiologist to perform a valsalva maneuver (PEEP ventilation) [113].
For small defects free autogenous mucus grafts are preferred, the majority of surgeons place the graft in an onlay /overlay technique [191], [195], [222]. When forming a graft one can expect approximately 1/5 shrinkage, the borders of the defect need to overlap at least 4mm even in case of small leaks [222], [232]. The correct orientation and position of the free mucosa graft has to be carefully taken into account - otherwise an intracranial mucocele (-cele = Ansammlung) may develop [233].
Postoperatively the patient has to be closely monitored. Especially the state of consciousness needs to be mediated closely - in case of loss of consciousness a neurosurgical consult has to take place immediately. ... After the complication-prone procedure, a postoperative CT scan [76], [135] is appropriate. If an instrumental penetration into the intracranial space as part of the genesis of the CSF fistula could not be clearly excluded, a CT scan is performed emergently and mandatory.
Complementary treatment - antibiotics
Complementary treatment - lumbar drains
Prognosis
A meta-analysis showed no significant difference regarding success rate, stating that revision surgery is generally performed in about 90% of all cases for small defects to up to 97% [72], [191], [203], [212], [221], [226], [227], [244]. Recurrence of fistulas is frequently observed in patients with an increased CSF pressure [231].
Active CSF fistulas may result in meningitis.
In a few cases (0.3 to 0.9%) perioperative complications are reported, such as
... In rhino-neurosurgery, the often extensively reconstructed dura represents a weak spot in the therapeutic concept. Originally, in up to 40% of the cases, postoperative fistulas were observed. This fact led, amongst others,
(of, characterized by, or containing cells or vessels that carry or circulate fluids, such as blood, lymph, or sap, through the body of an animal or plant)
(a footlike, stemlike, or narrow basal part or structure, such as a narrow strip by which a graft of tissue remains attached to the donor site.)
(= flaps composed of mucous membrane and periosteum, as from the hard palate or gingiva)
A number of special factors determine the particular risk associated with a large dura deficiency:
In the majority of cases, especially for postoperative persisting heavy flow of cerebrospinal fluid, revision surgery is advisable [182].
An early drainage can help to relieve pressure variations within the area of transplantation during extubation [233]. In about 13% of the cases however, the drainage causes more or less relevant side effects or complications in time, e.g., [102], [261]
4.4 Synechiae, "missed ostium sequence", unstable middle turbinate with lateralisation
4.5 Hyposmia
In human anatomy the exact dimension of the olfactory region is unknown. It is formed [311], [312], [313] by an area consisting
In general, postoperative smell deficits may occur after direct mechanical trauma, after removal of olfactory mucosa accompanied by scarification of the latter, caused by a progressive inflammation of the mucosa or even by a postoperative modification of the nasal air passage. A partial resection of the lower third of the anterior middle nasal turbinate does not affect the ability to smell - in routine resections, there was no evidence of olfactory mucosa in the surgical specimens [314]. On the other hand, a complete postoperative anosmia was reported, following a resection of the superior nasal turbinate that was done by mistake [313]. Olfactory fibers in the turbinate bone can also be damaged without any resection, e.g. by mere fractures occurring in the context of a "mobilization" of the turbinates - however, because of the remaining septal fibers, a hyposmia and no anosmia could be expected [315].
Preoperatively, about 17% of the routine patient population suffering from chronic rhinosinusitis is affected by olfactory disorders. After surgery, many of these patients can expect an improvement or a normalization. 16% of patients suffering from preoperative olfactory disorders were not aware of their impairment. For medico-legal reasons, these circumstances suggest that a preoperative measure of olfactory ability should always be performed. For rough orientation purposes, the rate of a postoperative arising hyposmia is indicated at about 3%, whilst the rate of a postoperative smell deterioration is estimated at about 9% [316], [317].
4.6 Atrophic rhinitis
... an irritating crust formation, accompanied by a restricted nasal physiology, occurs in up to 33% of all cases [42], [102].
After extensive nasal surgery, secondary atrophic rhinitis may develop (Figure 4a).
Regarding treatment of mucociliary circuits (see above), in some cases a "mega antrostomy" is recommended [288]. Similar to "medial maxillectomy", excessive loss of concha tissue may occur, resulting in a dry nose.
In routine surgery of chronic rhinosinusitis, the rate of postoperative atrophic rhinitis is roughly between 0.08 and 0.4% [72], [98]. Therapy is mainly conservative, based upon intensive moistening, local care with the administration of ointments or oils [291], [320].
The internet offers patients affected by the "empty nose syndrome" (ENS) a special website: "Empty Nose Syndrome Self-Help Website"- here, the excessive resection of any turbinate tissue within routine sinus surgery is referred to as a "nasal crime".
[Tutorials and Tips
4.7 Nerve injuries - infraorbital nerve, alveolar nerve
In a rather aggressive mode of preparation or when electrosurgical measures are applied in the maxillary sinus, an injury of the infraorbital n. at the roof of the maxillary sinus may result.
... As a consequence, facial sensibility is affected postoper- ative [76], [288] (Figure 5). The same applies to the alveolar nerves. The rate of postoperative sensibility disorders of teeth or lips and cheeks respectively is about 3% for all cases combined [72].
In justified individual cases of endonasal procedures, a complementary, localized transoral puncture of the maxillary sinus is recommended in order to remove hyperplastic mucosa in hidden anatomical areas, e.g. via insertion of a shaver [25], [328]. Only about 3% of patients benefit from this procedure, its use within the scope of pansinus surgery in case of polyposis is questionable [53], [328]. In an adverse case, a branch of the infraorbital n., above all the superior alveolar n. is damaged [288]. In 3/4 of all cases, complications occur postoperatively, such as cheek swelling, face pain, numbness of the face or teeth or even paresthesia. In about 30% of patients, these complaints remain in part permanently, most likely as a local dysesthesia [328].
... In ...
transpterygoid (Pterygoid ist ein Knochen der hinteren Gaumenregion)
... rhino-neurosurgical approach, amongst others, the maxillary or the vidian n. can be damaged [182]. Consequential effects of the latter lesion corres- pond to those of a vidian neurectomy which often leads to a temporary reduction of the lacrimal secretion (xeroph- thalmia, postoperative incidence 12-30%) and reduction of the moistening of nasal mucous membranes [331], [332]. Past references depict single cases of severe or- bital complications of vidian neurectomy. Recent literature only reports occasional cases of e.g., combined injuries of the local trigeminal n. and sympathic n. with neurotroph- ic keratopathy, miosis and headaches after monopolar coagulation at the vidian n. [333].
5 Severe or threatening complications
5.1 Orbital haematoma
5.2 Relevant bleeding (anterior ethmoidal a., posterior ethmoidal a., sphenopalatine a. and internal carotid a.)
Injury of the anterior ethmoidal a.
The anterior ethmoidal a. can be easily injured during surgery of the anterior ethmoid.
Arteries at risk are those
If the artery has been injured and is bleeding into the ethmoidal cavity,
Injury of the posterior ethmoidal a.
The distance between the anterior and the posterior ethmoidal artery is approximately 10-14 mm and the distance from the latter to the optic nerve as well as to the anterior wall of the sphenoid is about 8-9 mm [12],. ...
Injury of the internal carotid a.
The distance between the internal carotid a. and the optic nerve is 2-10 mm, ... The exact incidence rate of carotid injuries in paranasal sinus surgery is unknown. According to literature, carotid artery injuries occur with a rate of 0.3% in surgery of diffuse chronic rhinosinusitis [72].
5.3 Reduced vision, visual field defects
The optic n. often bulges into the superior-lateral wall of the sphenoid sinus. In this regard, very different frequencies are found in literature: 8-100% [12].
5.4 Diplopia
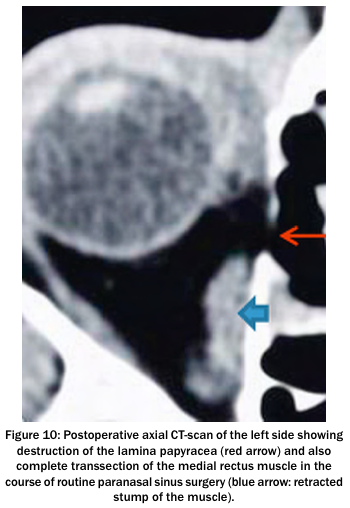
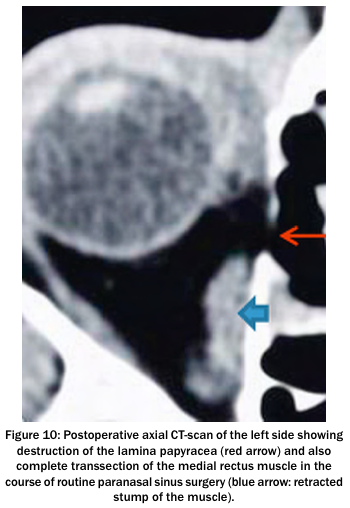
In endonasal surgery of the paranasal sinuses, an impairment of the medial rectus muscle (m) is likely to occur with an incidence of approximately 1/1000. In general, these injuries result of a fracture of the inferior lamina papyracea with perforation, destruction or incarceration of the muscle. The middle or posterior ethmoid is most at risk - as hardly any fat is situated between the muscle and the bony orbital wall [76], [104], [363], [449]. In rare cases, there is a particular risk due to a congenital or posttraumatic bulge of the lamina papyracea with or without direct embedding of parts of the muscle [107], [450].
Other eye muscles are distinctly less often injured intraoperatively:
The inferior rectus muscle may be damaged in surgeries involving the maxillary sinus and
the superior oblique (trochlea) muscle may be lacerated in extended endonasal frontal sinus surgery with a drill for instance.
Injuries of the inferior oblique m. have also been described [71], [76], [104], [363], [451], [452], [453].
In the majority of cases, only one eye muscle is damaged, with a relevant orbital hematoma developing additionally in one quarter of patients. Occasionally, however, severe combined damage affecting three muscles, for example, has been observed with additional bleeding, retinal damage or lesions of the optic nerve (n). or of the oculomotor n. [104], [453], [454].
Generally 5 typical causes for a postoperative motility disorder of the eye may be distinguished:
1. Partial or complete transection of the muscle.
2. Contusion with hematoma of the muscle tissue.
3. Impairment of the oculomotor n., e.g. at the point of transition between the middle and the dorsal third of the medial rectus muscle.
4. Prolapse and incarceration of muscle parts and/ or fat into a defect of the orbital wall.
5. Destruction of intraorbital fascia with irregular scarring ("fat adherence syndrome") [363], [453], [455], [456].
Very often (50%), eye muscle damage is not noticed intra-operatively by the surgeon [453]. Muscle tissue that is quickly destroyed through the 'shaving action'. This may also occur without any prominent orbital injury. Often the surgeon is not even aware of the damage.
... Two to three months after a damage caused to the medial rectus m., strabismus surgery is indicated [116]. In two thirds of cases, several operations will be necessary [358], [458]. In the majority of cases after an ophthalmic surgery, ocular functional deficits remain, although most of the patients (90%) are satisfied with their eye sight function in daily life [451], [455], [458].
The perforation in the lamina papyracea may be difficult to identify, even in postoperative imaging [17], [71], [363], [449], [459].
In other cases, motility limitations can be distinctly higher than the damage seen at imaging. Here, diffuse deformities, known as "fat adherence symptom" (see above) are assumed to evolve, together with a 'de-compartmentalization' of the extraconal fat tissue, followed by adhesions between the periorbit, fat, sclera and extraocular muscles [17]. After injuries caused by the shaver, chances to reconstruct the medial rectus muscle successfully are rather limited [340].
In rhino-neurosurgical operations, especially in the parasellar and suprasellar region (http://medical-dictionary.thefreedictionary.com/sella), in the area of the cavernous sinus or the clivus, thermal injuries or transections may lead to injuries of the abducens n. or the oculomotor n.. Frequently the oculomotor nerve recovers postoperatively from damages as long as the continuity of the nerve is preserved [102].
5.5 Enophthalmos
5.6 Lacrimal duct injury, complications of endonasal dacryocystorhinostomy
Epiphora (Tränenaustritt) develops in about 0.1 to 1.7 % of cases after sinus surgery [71], [98], [480], [481]. Inapparent injuries of the lacrimal ducts are described in 3% of cases (in individual cases up to 15%). Under favorable circumstances, such cases correlate with an unintended dacryocystorhinostomy [480], [481], [482] (Figure 11). An injury mostly occurs during infundibulotomy (uncinectomy), during surgery on the anterior frontal recess or during maxillary sinus fenestration in the anterior middle nasal passage - in the latter, particularly during the use of the backward cutting punch [71], [288].
The effectiveness of endonasal dacryocystorhinostomy [Tränenabfluss-Chirurgie] is undisputed, experienced surgeons have a success rate of more than 85% [483], [484]
5.7 Skull base injury, tension pneumocephalus, encephalocele [Hirnteile wölben sich nach außen]
... Symptoms are
If the underlying process is not interrupted,
... After the diagnosis has been confirmed in the emergency CT scan, immediate neurosurgical decompression has to take place, e.g. by trepanation or performing a puncture, with simultaneous closure of the skull base defect [491], [496].
5.8 Meningitis, brain abscess, intracranial haemorrhage
Meningitis, brain abscess [umschriebene Eiteransammlung im Gehirn nach durch Entzündung bedingtem Untergang u. Verflüssigung ("Einschmelzung") von Hirngewebe]
Postoperative meningitis is rare, although it represents the most frequent intracranial complication in paranasal sinus surgery. It spreads through
... In rhino-neurosurgical procedures, the postoperative rate of meningitis is about 1-3% [102], [237], [248], [501], [502]. Risk factors are
On the contrary earlier irradiation, the patient's age, pathology, or the duration of a lumbar drainage do not affect the rate of meningitis.
Most studies imply that prophylactic administration of antibiotics does not reduce the risk of meningitis or brain abscess in skull base surgery [503].
Subdural hematoma, cerebral hemorrhage, ischemia
Uncomplicated cerebrospinal fluid fistulas ... may lead to severe complications, e.g. by means of suction of tissue into the skull base defect,
Instantaneous fatal bleeding can possibly occur due to an injury of the internal carotid a., the anterior cerebral a. or the anterior communicating a..Serious damage can also be triggered by induced arterial spasms [90]. The defect at the skull base can cause a secondary herniation of brain tissue [518]. An iatrogenic encephalocele can develop slowly within months and might only become apparent though meningitis [200]. After extensive reconstruction of the frontobasal region and after a large amount of CSF has been discharged, intracranial pressure may drop, which in turn can result in displacement of the graft or tension on the bridging veins causing a subdural haematoma. For these reasons, a lumbar drainage is contraindicated in case of a prominent pneumocephalus. After extensive surgical procedures, a CT control must be performed on the first or second postoperative day [251].
5.9 Direct mechanical cerebral trauma, severe combined injuries
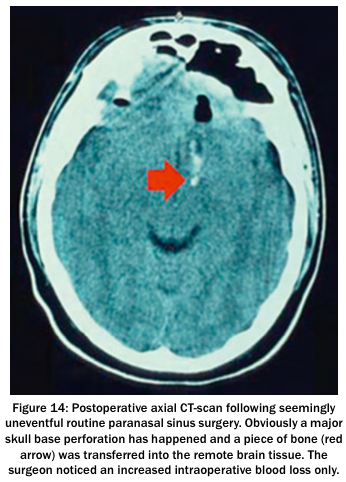
Fatal, partially lethal complications with mechanical destruction of cerebral tissue are limited to extremely rare cases in routine paranasal sinus surgery. Corresponding reports are mostly from earlier decades [349], [519]. In individual cases, severe combined injuries of brain and vessels can occur, e.g. with a traumatic aneurysm of the anterior cerebral a. [198]. Smaller case series report a clustering of corresponding incidents, partly on the right hand side and partly on the left hand side [520], [521]. Intraoperatively, the surgeon is mostly not aware of life- threatening brain damage, often only a "striking bleeding tendency" is registered (Figure 14). The removal of "indistinct tissue" for histological analysis, which then turns out to be orthotopic cerebral tissue, is tragic. ... Serious injury patterns have also been induced accidentally with the shaver [ = rotation suction knife was developed in beginning 1985 in orthopedic surgery. In the field of otolaryngology it was used in 1992-1994].
5.10 Toxic shock syndrome
In a large number of cases the initial source is nasal packing. The incidence of TSS in nasal surgery is indicated with 16/100,000. Rare cases have occurred in connection with the use of septum foils, due to a special post- operative formation of crusts or following chronic or acute rhinosinusitis without any abnormalities [528], [529], [530], [531].
5.11 Anosmia
The rate of postoperative anosmia as a complication of sinus surgery is about 0.07% to 1% [72], [534]. Altogether, the rate of postoperative anosmia is approximately 2% [326], [393]
Version: 12.5.2016
Address of this page
Home
Joachim Gruber